Platelets, Haemostasis and Blood Coagulation
Created by Khin Soe.
PLATELETS: STRUCTURE AND COMPOSITION
Platelets (small plates), also known as thrombocytes, (thrombo = clot; cytes = cells) have following features:
Size
Platelets are the smallest blood cells varying in diameter from 2 to 4 μm with an average volume of 5.8 μm3.

Shape and colour
Platelets are colourless, spherical or oval discoid structures.
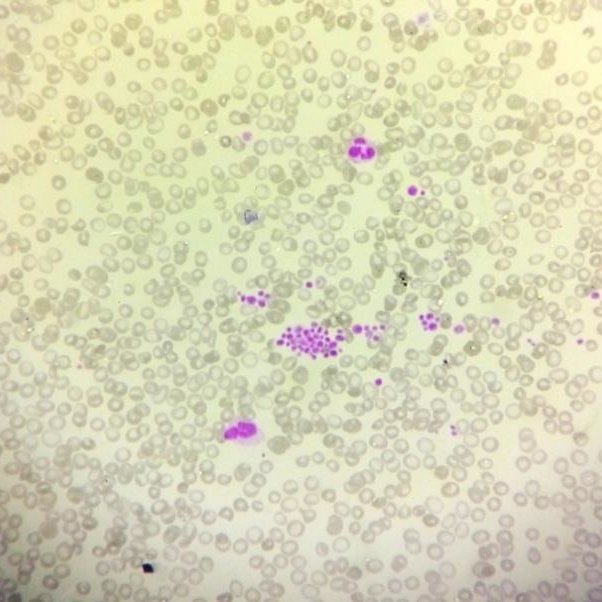
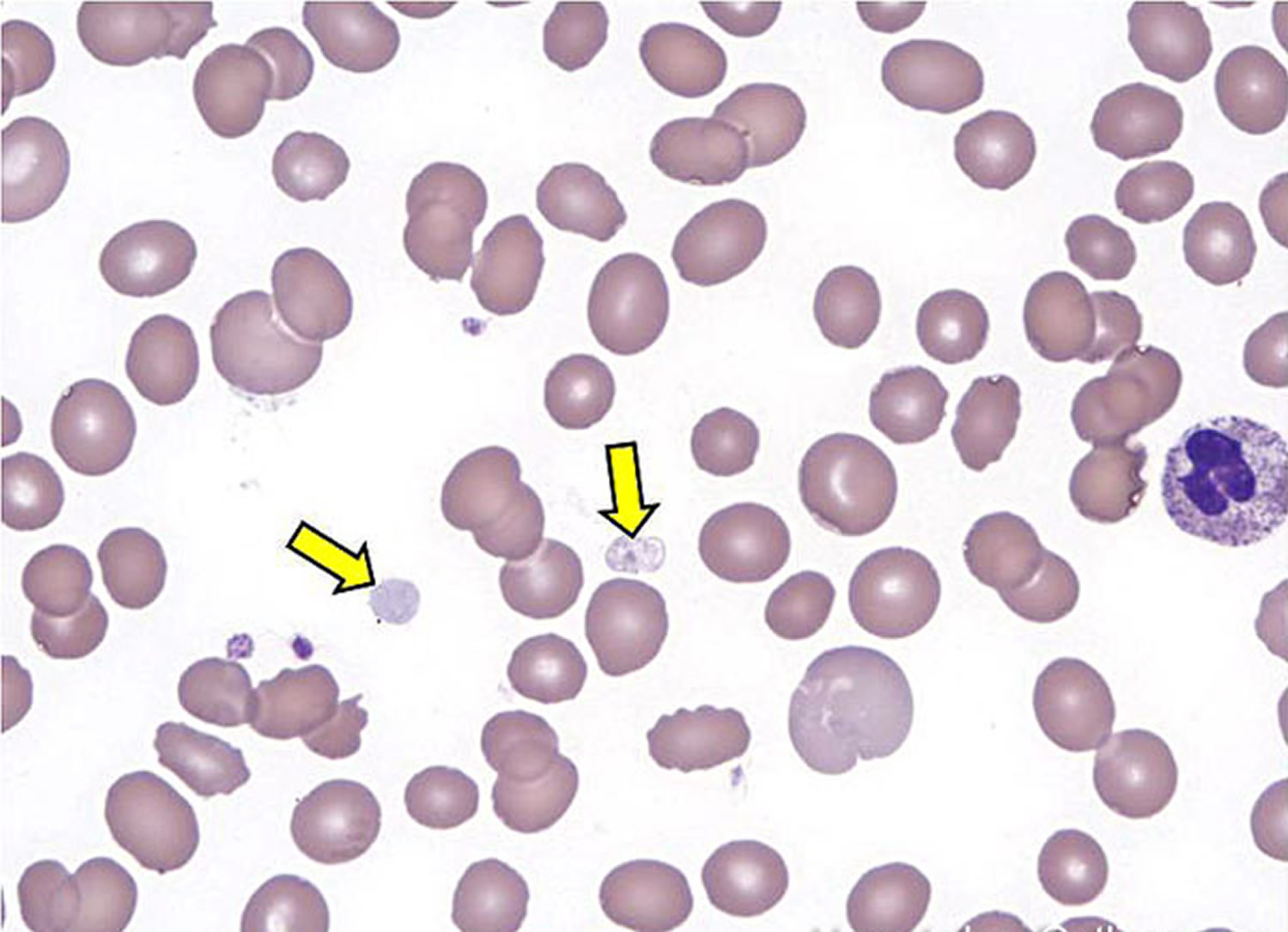
Leishman staining
Leishman staining shows a platelet consisting of faint bluish cytoplasm containing reddish purple granules.
Nucleus
Nucleus is absent in the platelets and therefore these cannot be reproduced.
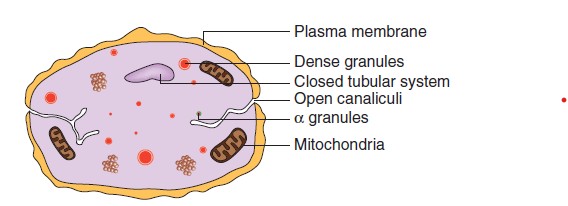
Electron microscopic structure
Under electron microscope a platelet shows following structural and compositional characteristics
Cell membrane: Glycoproteins
Glycoproteins forming the surface coat of the platelet membrane prevent adherence of platelets to normal endothelium

Cell membrane: Glycoproteins
but accelerate the adherence of platelets to collagen and damaged endothelium in injured blood vessels.
Cell membrane: Phospholipids
Phospholipids of the platelet membrane contain platelet factor-3, which plays an activating role at several points in the blood clotting process.
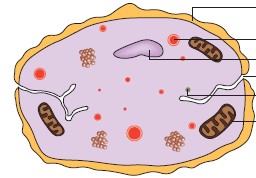
canalicular system or the surface connecting system
Invagination of the surface membrane forms the socalled canalicular system or the surface connecting system.
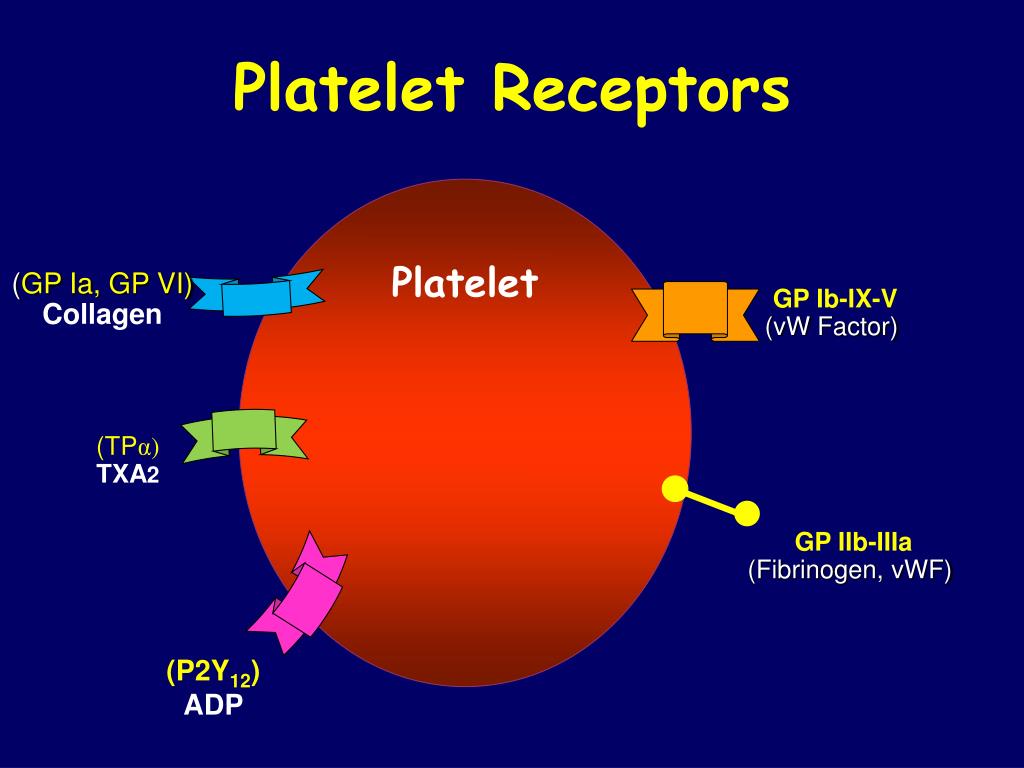
Receptors
Receptors present on the platelet membrane are meant for combining with specific substances like collagen and fibrinogen.
Precursors
Precursors of various substances like thromboxane A2, prostaglandins, leukotrienes and platelet factors 3 and 4 are also present.
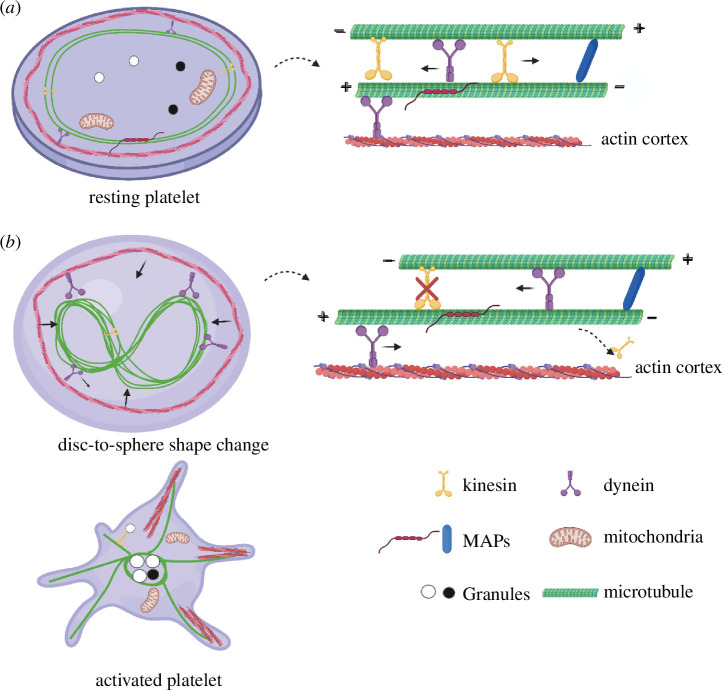
Microtubules
These form a compact bundle present immediately beneath the platelet membrane, responsible for maintenance of discoid shape of the circulating platelets.
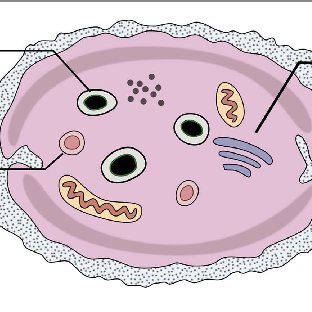
Cytoplasm
Proteins and Granules: Fibrin stabilizing factor, – Platelet-derived growth factor (PDGF) and – Von Willebrand factor, - serotonin (5HT), - Clotting factors and PDGF.
Properties of platelets
Adhesiveness: when they come in contact with any wet surface or rough surface, they get activated and stick to the surface.
Adhesiveness
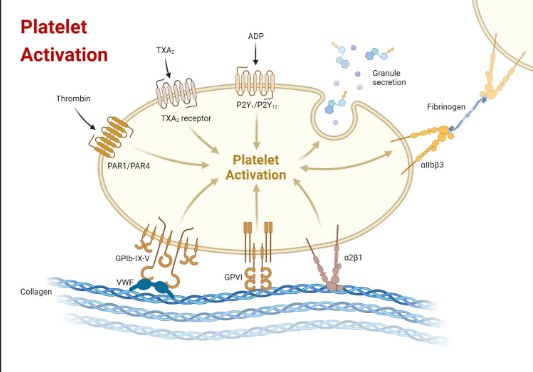
Factors responsible for adhesiveness are collagen, thrombin, ADP, thromboxane A2, calcium ions and von Willebrand factor.
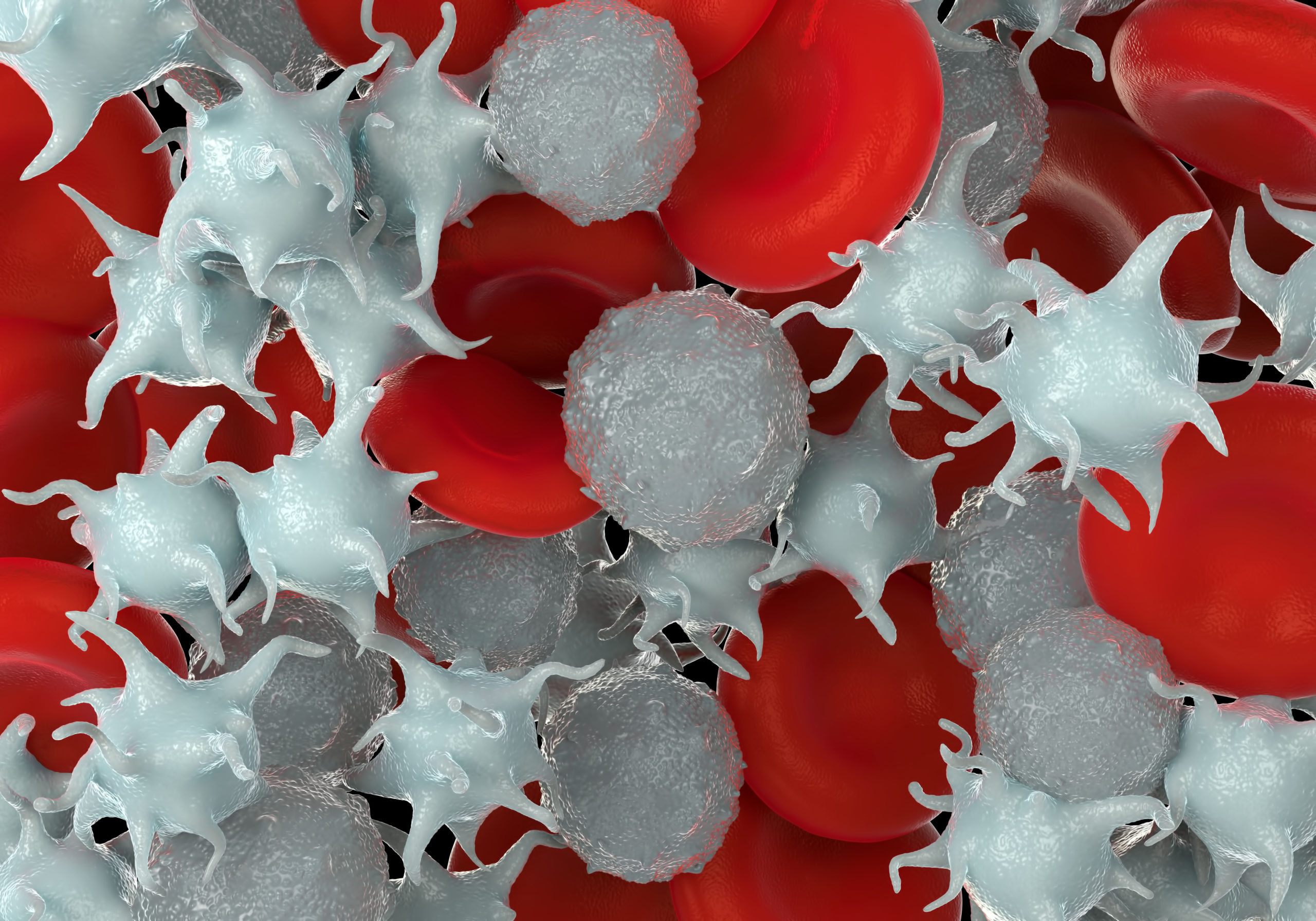
Aggregation of platelets
Platelets have the property to aggregate, i.e. they stick to each other. This is due to ADP and thromboxane A2.

Agglutination of platelets
Clumping together of platelets is called agglutination. This occurs due to the actions of some platelet agglutinins.
Functions of platelets
Role in haemostasis. Haemostasis refers to the spontaneous arrest of bleeding from an injured blood vessel. Platelets play roles in haemostasis.
Role in clot retraction
Contraction of contractile proteins (actin, myosin and thrombosthenin) present in the platelets play an important role in clot retraction.
Normal count
Normal platelet count ranges from 150,000 to 450,000/mm3, with an average count of 2.5 lakh/mm3.
Pathological variations
Thrombocytosis. An increase in the number of platelets more than 4.5 lakh/mm3 is called thrombocytosis.
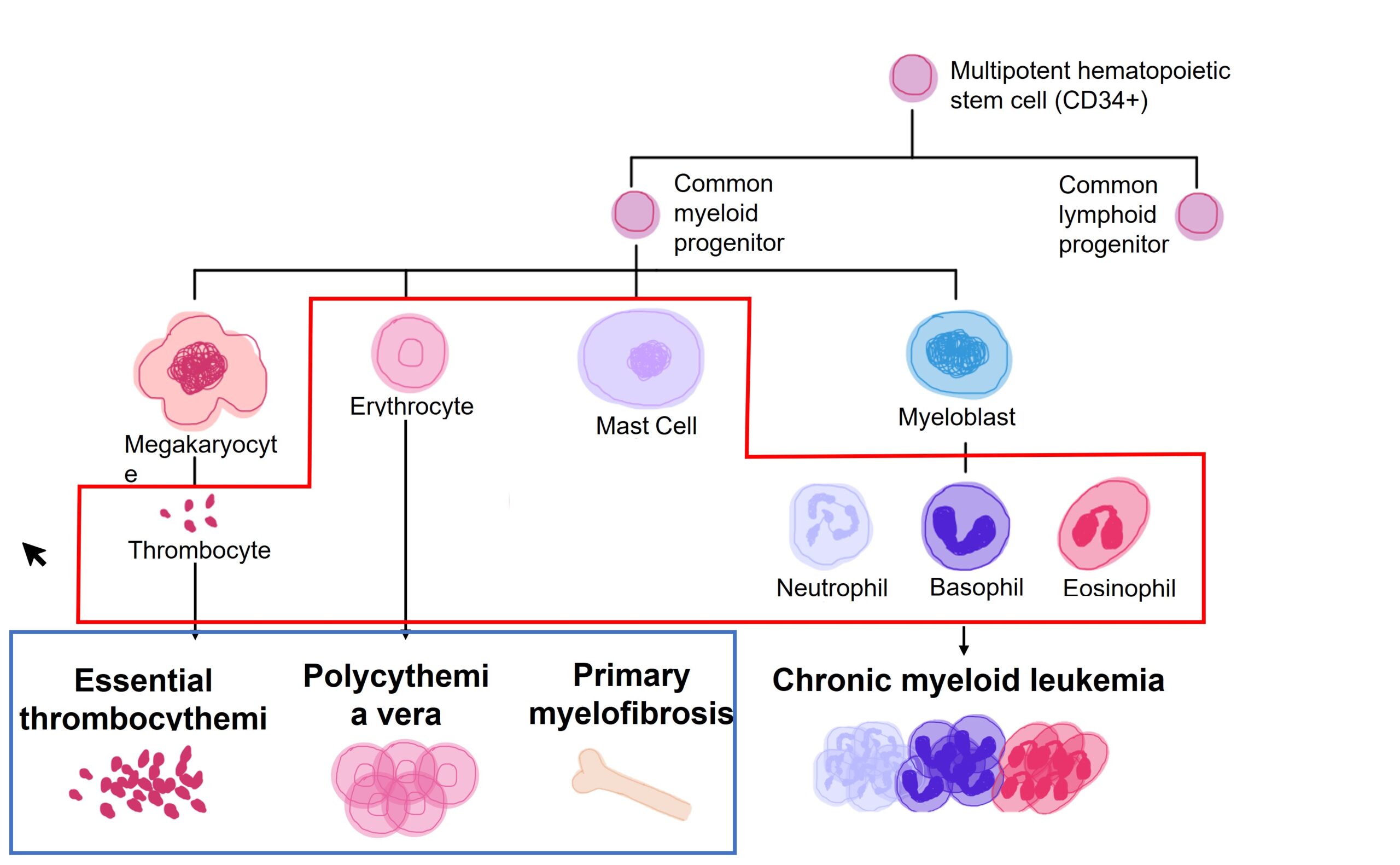
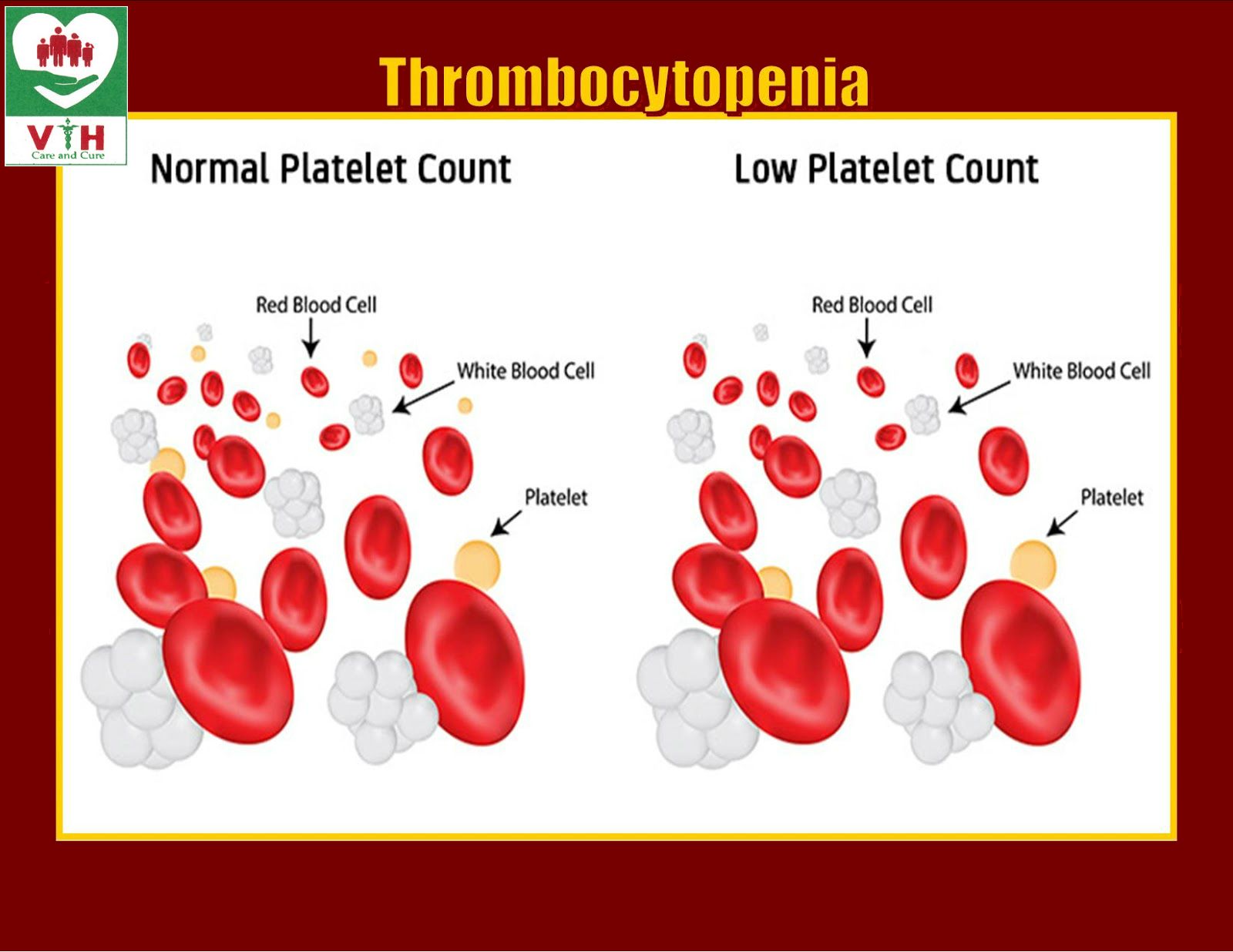
Thrombocytopenia
Decrease in the number of platelets below 1.5 lakh/mm3 is called thrombocytopenia.

Causes of Thrombocytopenia
Idiopathic thrombocytopenic purpura
Causes of Thrombocytopenia
Acute leukaemia or secondary deposits of malignancy in the bone marrow
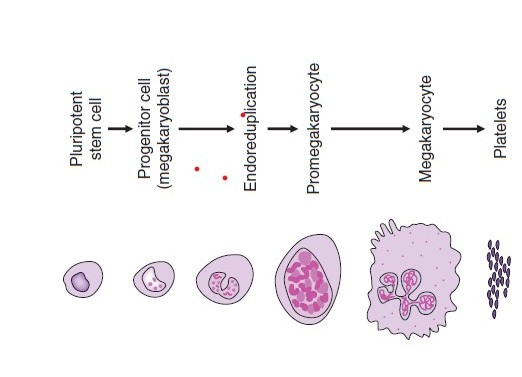
Stages of thrombopoiesis
Control of thrombopoiesis
Thrombopoiesis seems to be regulated by following humoral factors: Thrombopoietin and Megakaryocyte colony stimulating activity (Meg-CSA).
Life span and fate of platelets
Life span of platelets varies from 8 to 12 days with an average of 10 days. Platelets are destroyed by tissue macrophage system in spleen.

HAEMOSTASIS
Haemostasis refers to the spontaneous arrest or prevention of bleeding from the injured/damaged vessels by the physiological process.
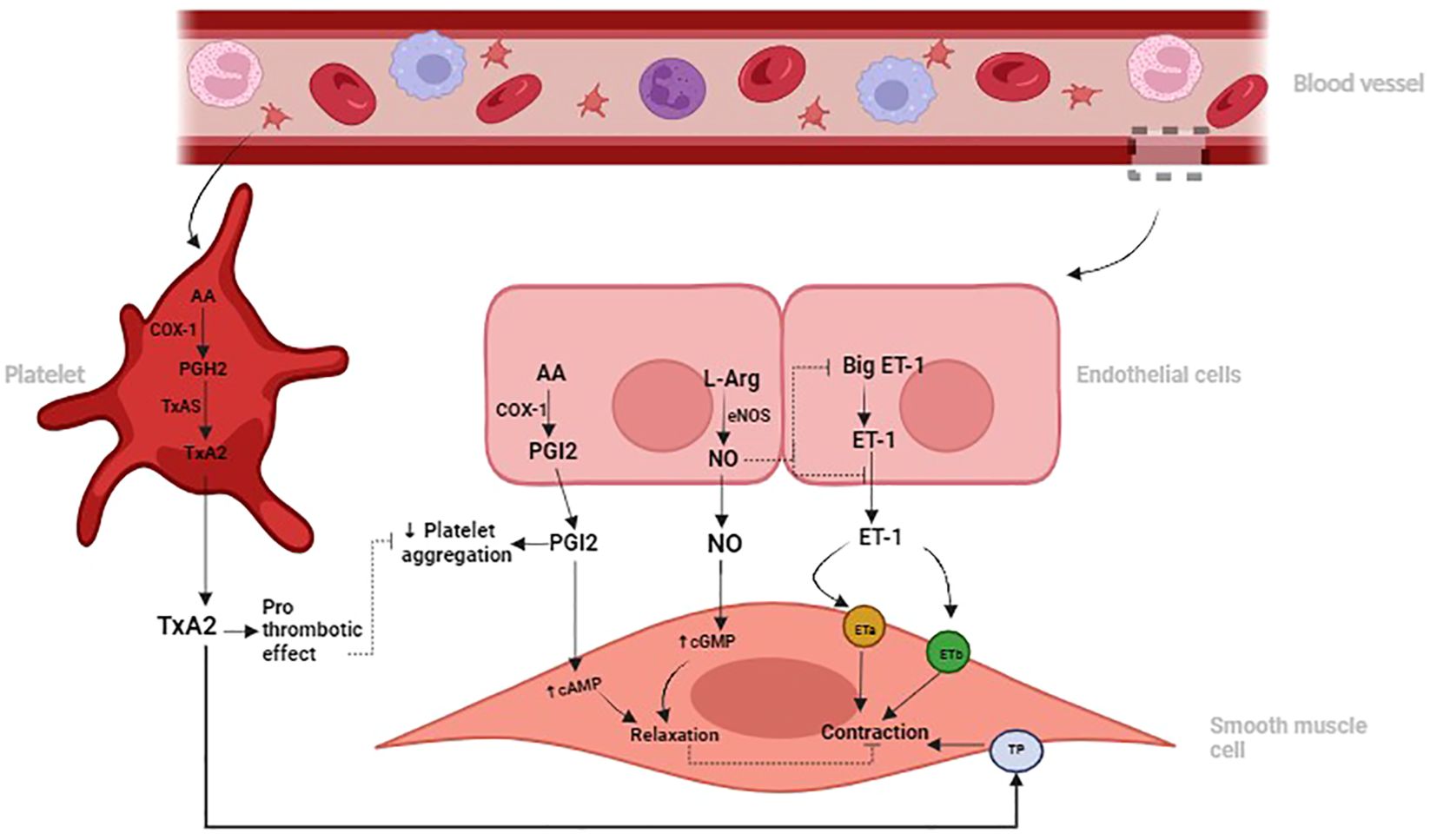
1. Vasoconstriction
Initial vasoconstriction is caused by direct effect of injury on the vascular smooth muscles. The initial vasoconstriction is transient but
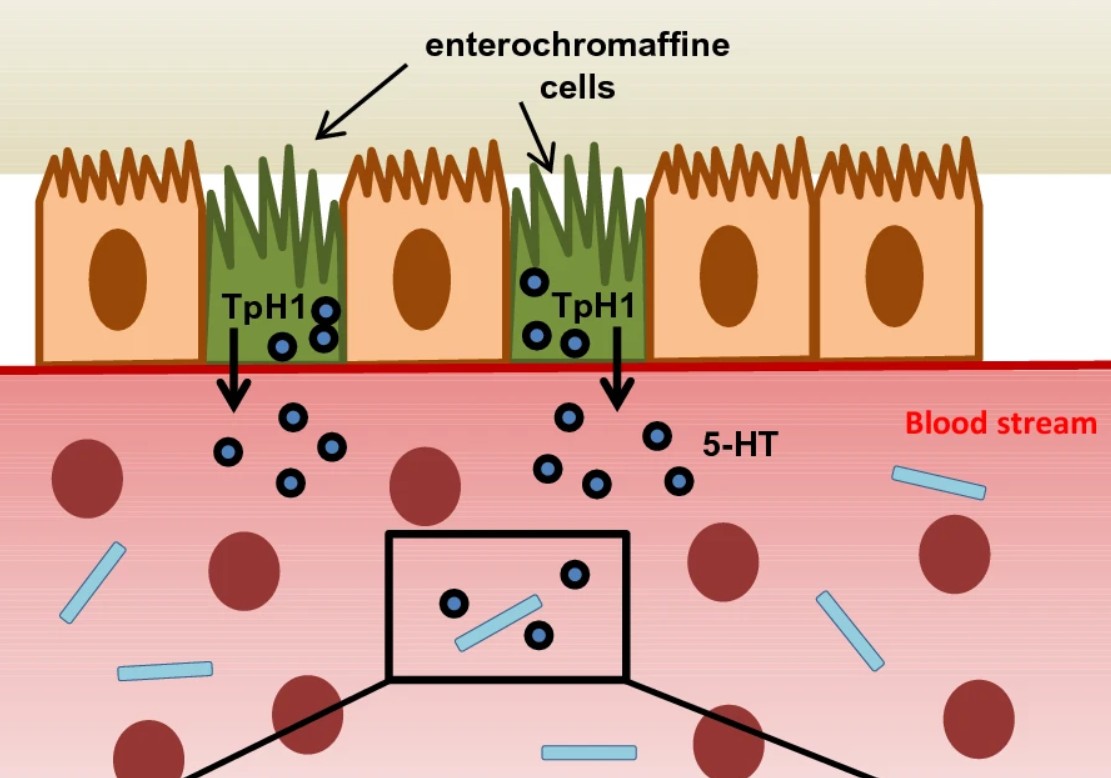
Serotonin (5-HT)
Enterochromaffine cells (EC-cells) in the gut express Tph1 and synthesize the majority of peripheral serotonin (5-HT). EC-cells release 5-HT into the blood plasma, where it is taken up by platelets.
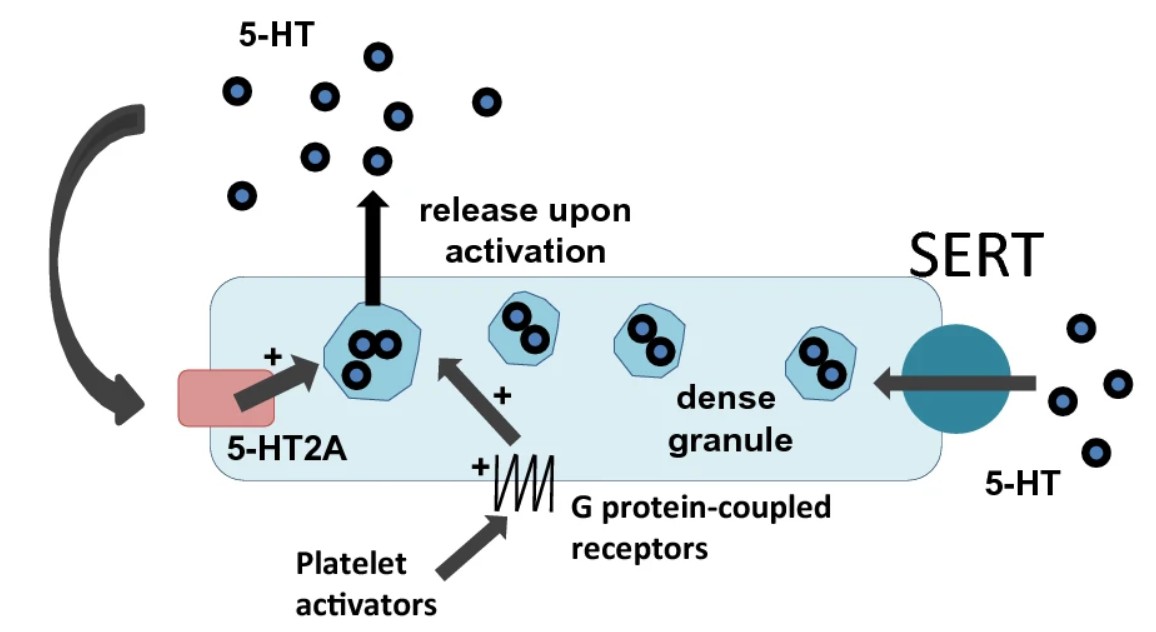
Serotonin (5-HT)
Platelets, as the main circulating reservoir, store 5-HT in their dense granules.
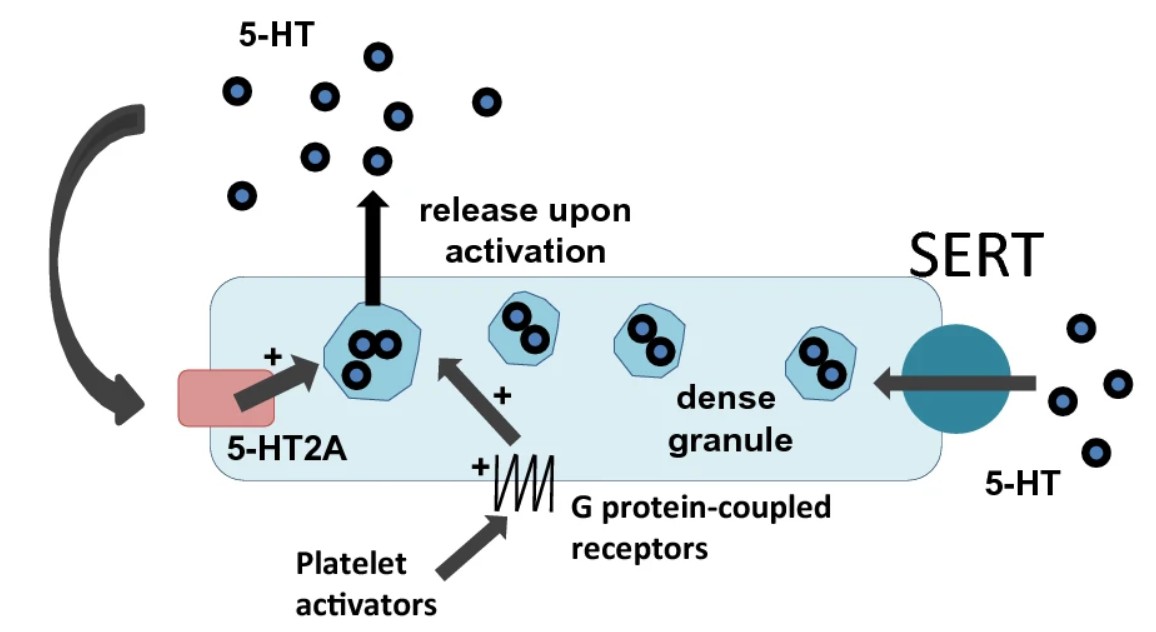
Serotonin (5-HT)
Platelets, as the main circulating reservoir, store 5-HT in their dense granules.
1. Vasoconstriction
is maintained for several minutes or even hours by humoral facilitation due to release of 5HT and other vasoconstrictors.
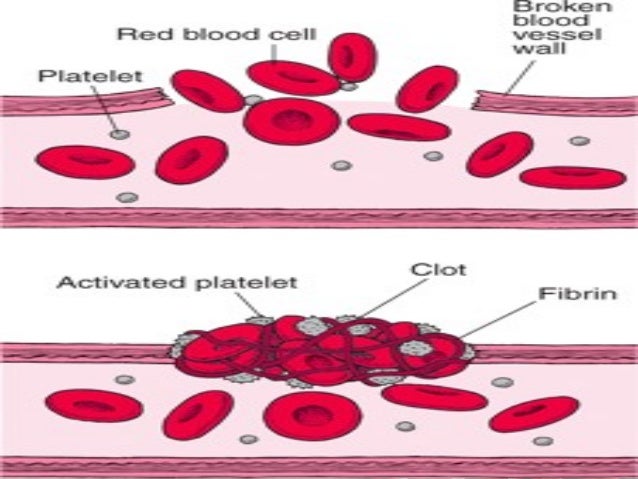
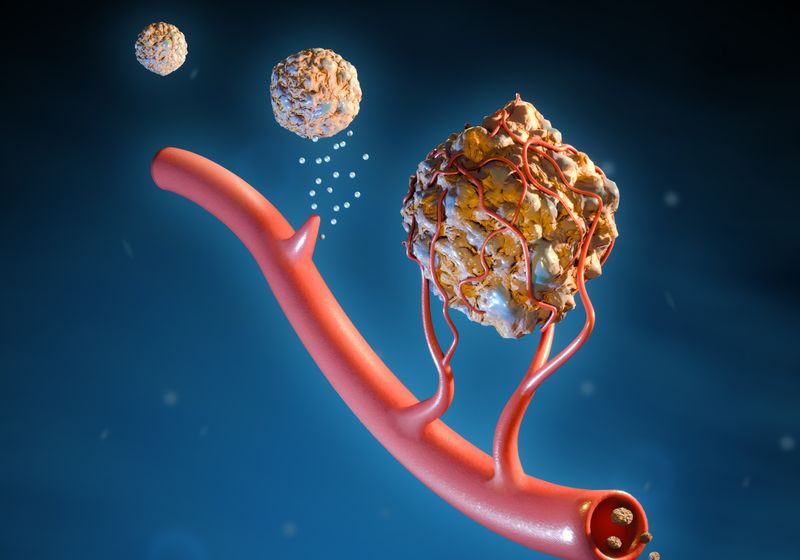
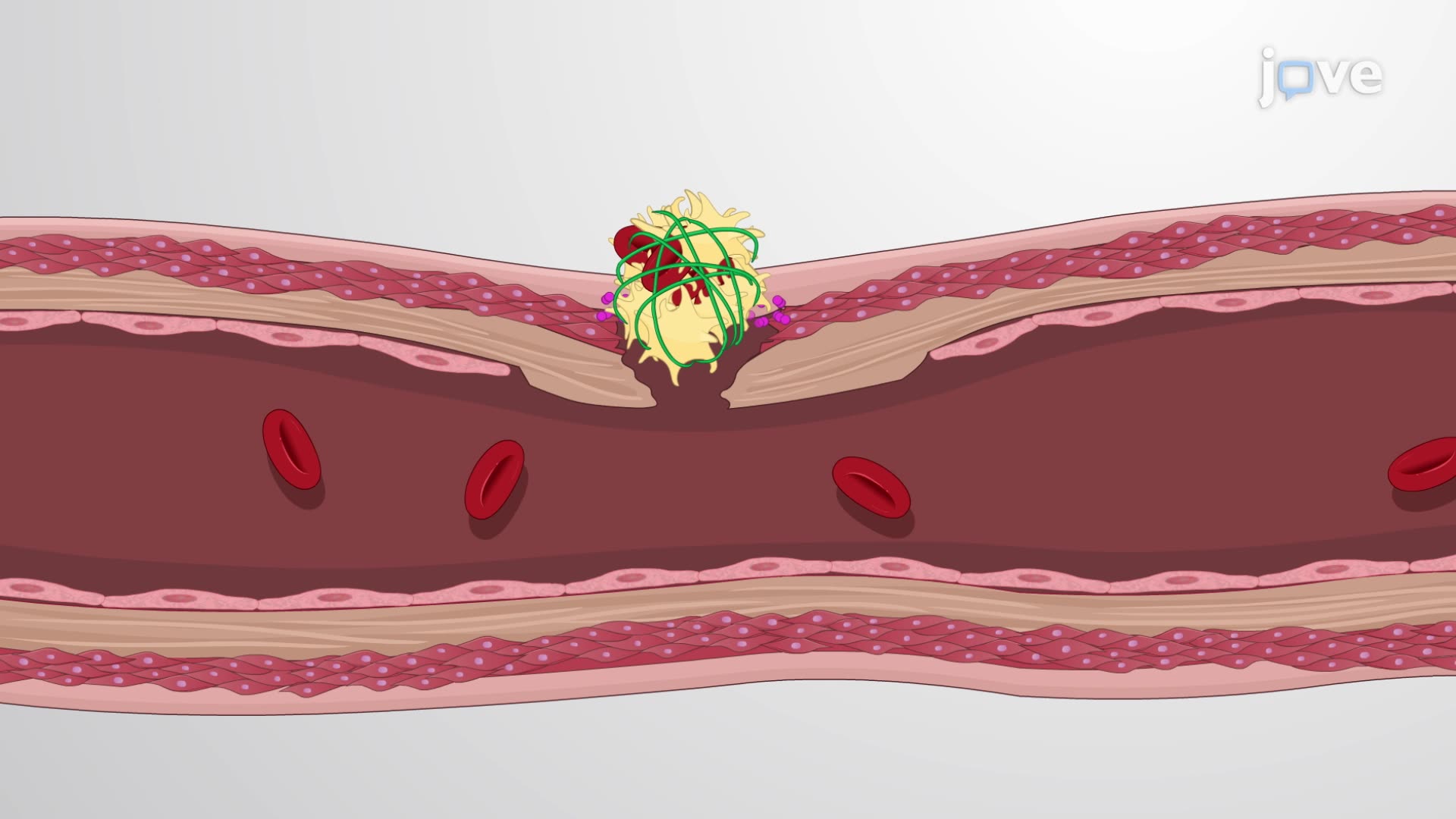
2. Formation of temporary haemostatic plug
Platelet adhesion. Following injury platelets become sticky and therefore adhere to the collagen of damaged cell wall and to the damaged endothelium.
Formation of temporary haemostatic plug
Platelets activation. The platelets secrete large quantities of ADP and thromboxane A2, which act on the nearby platelets and cause their activation.

2. Formation of temporary haemostatic plug
Platelets aggregation. The large numbers of activated sticky platelets stick to each other forming platelets aggregation.

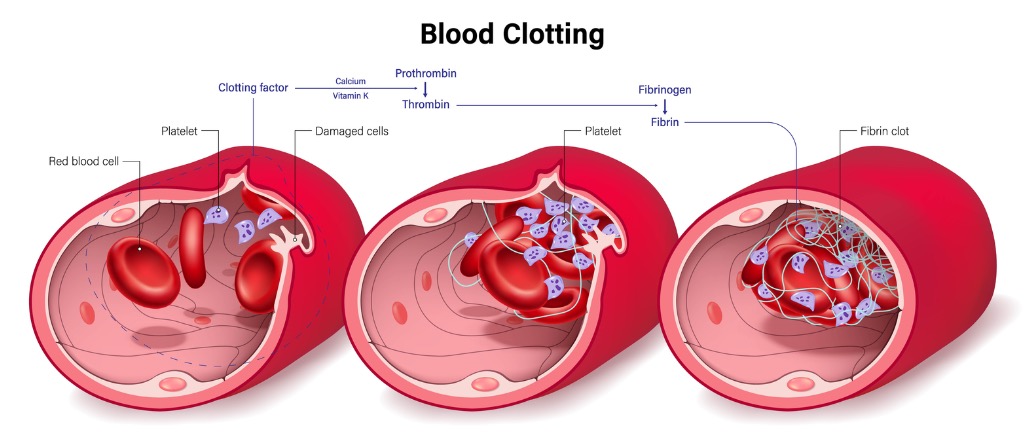
3. Formation of definitive haemostatic plug
The temporary platelet plug is converted into the definitive haemostatic plug by the process of clot formation (blood coagulation).
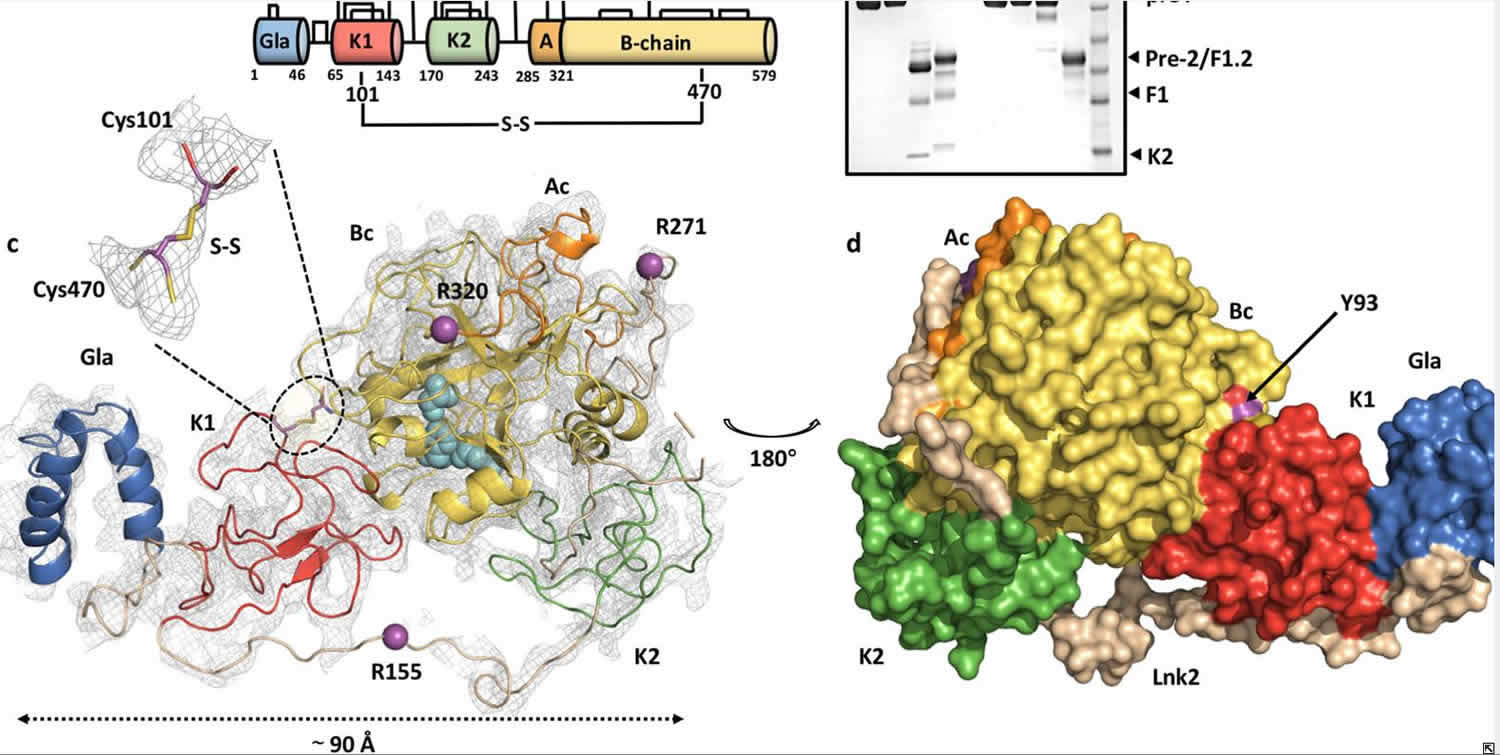
3. Formation of definitive haemostatic plug
Platelets play an important role in the formation of the intrinsic prothrombin activator which is responsible for initiating the process of clot formation.

BLOOD COAGULATION
When the blood is shed from the blood vessels or collected in a container, it looses its fluidity within a few minutes and

BLOOD COAGULATION
gets converted into a jelly-like mass called clot. This phenomenon is called coagulation or clotting of blood.
BLOOD CLOT RETRACTION
Within a few minutes after a clot is formed, it begins to contract and usually squeeze out most of the fluid called serum (plasma without fibrinogen and other clotting factors) within 30–60 min.
Contraction is activated by thrombin and calcium ions
The contractile proteins (platelet thrombosthenin, actin and myosin) present in the cytoplasm of platelets cause strong contraction of platelet spicules attached to fibrin fibres.
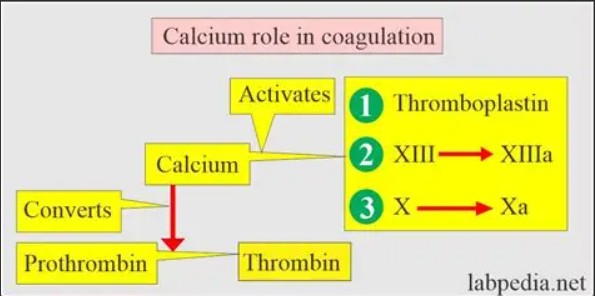
Role of vitamin K
In the liver, synthesis of following factors is dependent upon vitamin K: Coagulant like prothrombin, Factors VII, IX and X, and Circulatory anticoagulant protein.
WHY CIRCULATING BLOOD DOES NOT CLOT?
1. Velocity of circulation. Blood is pumped into the vessels and circulated at a constant velocity, which contributes to its fluidity.
2. Surface effects of endothelium
Smoothness of the endothelial lining inhibits platelet adhesion.
2. Surface effects of endothelium
A layer of glycocalyx (mucopolysaccharide) adsorbed to the inner surface of endothelium being negatively charged repels clotting factors (anion proteins) and platelets, and thereby prevents clotting.
2. Surface effects of endothelium
Intact endothelium acts as a barrier between the thrombogenic subendothelial collagenous tissue and the blood.
2. Surface effects of endothelium
Intact endothelium acts as a barrier between the thrombogenic subendothelial collagenous tissue and the blood.
3. Circulatory anticoagulants
Circulatory anticoagulants or the so-called natural anticoagulants present in the blood which prevent clotting are: Heparin, Antithrombin III, α2 macroglobulin and Protein C.
4. Fibrinolytic mechanism
Protein C is a naturally occurring anticoagulant which inactivates factors V and VIII and also inactivates an inhibitor of tissue plasminogen activator.

5. Removal of activated clotting factors
Liver plays a role in preventing the intravascular clotting by removing activated clotting factors in the event of onset of spontaneous clot formation.
THROMBOSIS
Under certain pathological conditions the intravascular clotting may occur. The intravascular clotting is called thrombosis and the clot so formed is called thrombus.
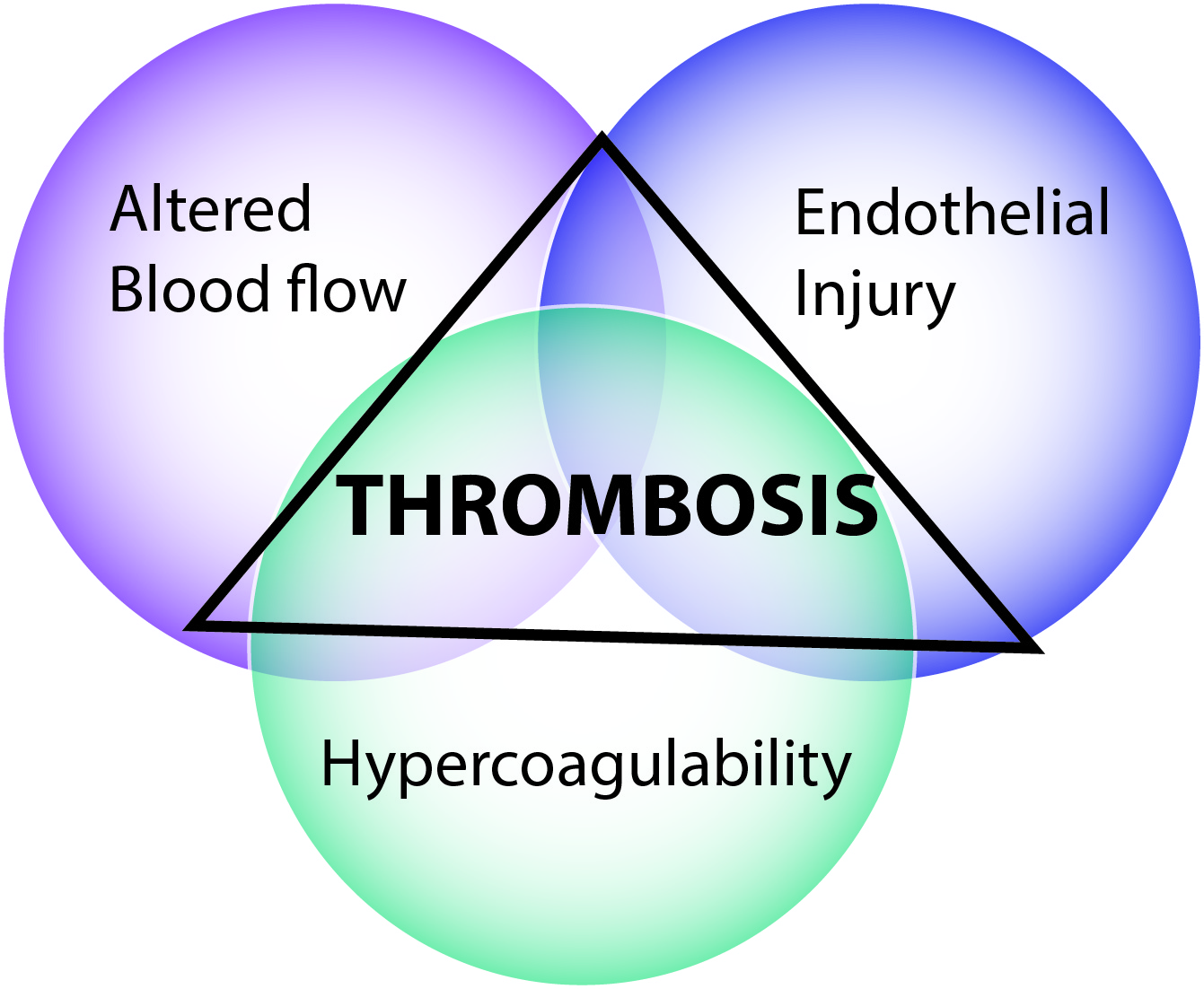
Predisposing factors of thrombus formation
Effects of thrombi
1. Ischaemia and infarction.
Effects of thrombi
Pulmonary embolism and Cerebral embolism.
